Scientists at the University of California-Riverside think they know why patients with multiple sclerosis (MS) are up to six times more likely to suffer from epilepsy. The newfound link may lead to the development of new therapies for both conditions.
Their study, “Chronic demyelination-induced seizures,” appeared in the journal Neuroscience. The mechanism underlying the increase in seizures in MS patients — a result of abnormal hyperactivity in nerve cells — has remained elusive.
Using a mouse model for MS, scientists discovered that one possible reason is the loss of myelin, a process known as demyelination. Myelin is a protective and conducting insulator layer surrounding the axon of nerve cells. A particular set of neurons, called parvalbumin interneurons and responsible for controlling neuronal hyperactivity, were particularly susceptible to myelin loss.
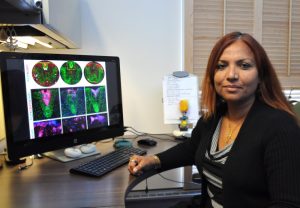
“Demyelination causes damage to axons and neuronal loss, specifically parvalbumin interneurons, are lost in mice, hyperactivity is no longer down but up, and this could be a cause of seizures,” Seema Tiwari-Woodruff, the study’s lead author and an associate professor of biomedical sciences at the UC-Riverside School of Medicine, said in a press release. “It’s very likely this is what is occurring in those patients with MS who are experiencing seizures.”
Researchers induced demyelination in mice by introducing into their diet cuprizone, a copper-binding substance that targets and damages myelin-producing cells called oligodendrocytes. After ingesting cuprizone for nine weeks, the mice started having seizures.
“Without myelin, axons are vulnerable,” Tiwari-Woodruff said. “They develop blebs — ball-like structures that hinder transport of important proteins and conduction of electrical signals. In some instances, significant axon damage can lead to neuronal loss. In both MS and our mouse model, parvalbumin interneurons are more vulnerable and likely to die. This causes the inhibition to be removed and induce seizures. Thus axonal and neuronal survival may be directly tied to the trophic support provided by myelin.”
When researchers removed cuprizone from the animals’ diet, the process of remyelination began and oligodendrocytes started to repopulate the demyelinated areas. These results have prompted a set of several questions, which scientists hope to address in future research.


